Attorneys handling birth injury and medical malpractice cases frequently encounter questions surrounding hypoxic-ischemic encephalopathy (HIE) in newborns. As a pediatric neurologist with experience in both clinical care and medicolegal case review, I understand the importance of a thorough, objective, and evidence-based approach when evaluating these complex scenarios.
The Complexity of HIE Causation and Diagnosis
Neonatal encephalopathy, and specifically HIE, is a clinical syndrome that may present with altered consciousness, seizures, and abnormal tone or reflexes. Establishing causation in these cases is rarely straightforward. Multiple factors may contribute, and the timing of injury—whether antepartum, intrapartum, or postpartum—often remains a matter of debate.
Key elements that may be considered in the assessment include:
- Indicators of fetal distress: Fetal heart rate abnormalities, sentinel events (e.g., placental abruption), and evidence of fetal acidemia.
- Need for resuscitation: Low APGAR scores and interventions such as assisted ventilation or chest compressions.
- Clinical signs of encephalopathy: Ranging from mild lethargy to severe symptoms such as seizures.
It is important to emphasize that none of these features alone are diagnostic, and each must be interpreted in the broader context of the clinical scenario.
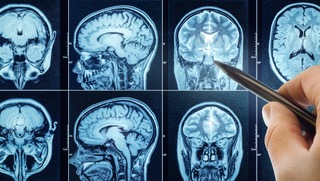
The Role and Limitations of Brain MRI
Brain MRI is commonly used to evaluate suspected HIE. It can reveal patterns that have been associated with hypoxic-ischemic injury, such as involvement of deep gray matter structures or cortical regions. However, MRI findings must be interpreted with caution:
- False negatives: Not all cases of clinical HIE result in abnormal MRI findings. Published literature notes that a significant minority of affected infants may have normal imaging, particularly if the scan is performed early.
- Timing and evolution: The appearance of injury on MRI can change over time. Early imaging may underestimate injury, while later scans can reveal evolving changes.
- Non-specific findings: Some MRI abnormalities may be seen in other conditions, including metabolic disorders, infections, or genetic syndromes.
MRI is a valuable adjunct, but it is not definitive for establishing causation or timing. A comprehensive assessment integrates imaging, clinical history, laboratory data, and other diagnostic information.
Conclusion
Determining the cause and timing of neonatal brain injury requires a careful, multidisciplinary approach. MRI is a powerful tool, but not infallible. Clinical, laboratory, and imaging findings must be integrated to reach a reasoned, evidence-based opinion. As an expert witness, my commitment is to provide objective, thorough analysis that supports the legal process without overreaching beyond what the science allows. You can contact me here.